Atrial Flutter
Atrial flutter is an arrhythmia caused by a macro-reentry circuit in the atria (most frequently located in the right atrium) that becomes a self-perpetuating loop.
During atrial flutter a very high-rated atrial impulse is originated —between 240 and 350 bpm— but, as in other types of supraventricular tachycardia, the heart rate (ventricular rate) is normally lower because the atrioventricular node is not usually capable of conducting impulses to the ventricle with such high rates.
Compared to atrial fibrillation patients, patients with atrial flutter are at similar risk for thromboembolic events, especially cerebrovascular accidents (strokes). Stroke risk must be estimated in every patient with atrial flutter n order to determine the need of oral anticoagulation treatment 1 2.
You can calculate stroke risk for patients with atrial flutter with our CHA2DS2-VASc score calculator.
Atrial Flutter on the Electrocardiogram
Atrial flutter is distinguishable on the electrocardiogram because it is a rhythmic tachycardia with heart rates that are divisors of 300 bpm, 150 bpm being the most frequent in untreated patients (AV conduction ratio 2:1).
There are no existing P waves, although atrial waves with “saw-tooth” pattern are spotted with rates around 300 bpm.
The QRS complex is narrow, except with previous bundle branch blocks or aberrant conduction (Ashman phenomenon).
In certain cases, it is arrhythmic and the conduction may be variable. As such, it can be mistaken for atrial fibrillation, but it is differentiated by the “saw-tooth” waves.
"Saw-tooth" Waves
This wave is characteristic of the atrial flutter, especially recognisable in the typical atrial flutter (see below).
It owns its name to its morphology in the EKG leads where it is predominantly negative.
Its main feature is a slow descending start, followed by a fast descending phase turning into a fast rise, finishing above the isoelectric line while connecting with the beginning of the following wave (creating thus the “saw-teeth” shape) 3.
It is usually visualised between the T wave and the following QRS complex. Also, it usually causes undulations of the isoelectrical segments, acting as a diagnostic aid in high heart rates.
Electrocardiogram Characteristics of Atrial Flutter
- Regular rhythm with heart rate around divisors of 300 (150 bpm, 100 bpm, 75 bpm).
- Absence of P waves.
- Waves in a saw-tooth pattern, with rates around 300 bpm.
- QRS similar to the preceding one, except aberrancy.
Types of Flutter:
Typical Atrial Flutter
It is the most common type. It is caused by a macro-reentry mechanism in the right atrium, where the stimulus runs in a loop.
Typical atrial flutter is easily recognised on the electrocardiogram by its well defined “saw-tooth” waves. By observing the inferior leads we can determine the direction of the stimulus and classify it further as counterclockwise atrial flutter or clockwise atrial flutter.
Typical Counterclockwise Atrial Flutter
The stimulus ascends through the interatrial septum to the roof of the right atrium, goes down the anterolateral wall and ends the circuit passing between the tricuspid valve and the inferior vena cava (cavotricuspid isthmus) reaching again the interatrial septum 3.
We can recognise it on the electrocardiogram by its well defined “saw-tooth” waves, which are negative in the inferior leads (II, III, and aVF).
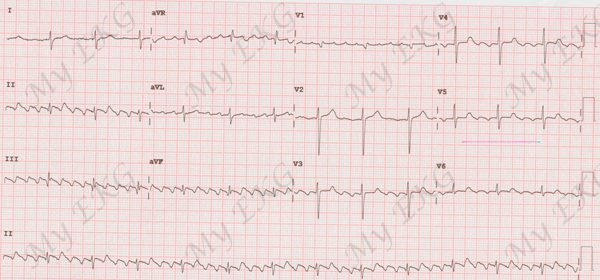
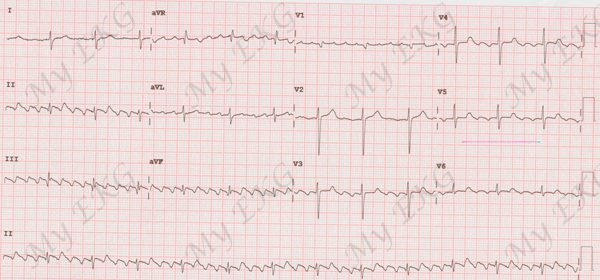
Typical counterclockwise atrial flutter:
Regular rhythm at 100 bpm with negative F waves in inferior leads.
Typical Clockwise Atrial Flutter
In 90% of the patients with typical atrial flutter the stimulus direction is as described above, but in 10% of patients the stimulus follows the opposite direction— that is, a clockwise direction.
On the electrocardiogram we observe well defined “saw-tooth” waves which are positive in the inferior leads (II, III, and aVF).
Atypical Atrial Flutter
It is less common than typical atrial flutter and even though it is also caused by a macro-reentry mechanism, this is produced in different structures as those described in the typical atrial flutter.
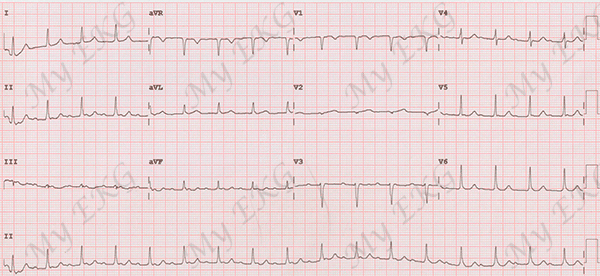
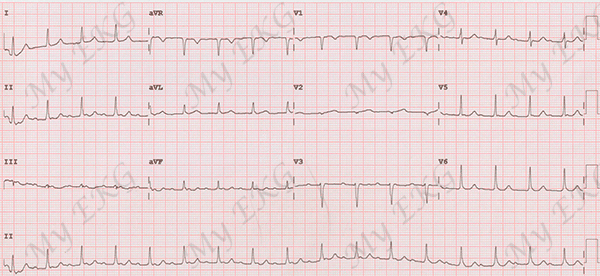
Atypical atrial flutter:
Regular rhythm at 100 bpm with small F waves resembling P waves, without “saw-tooth” waves morphology.
Atypical atrial flutter have less clear causes, sometimes secondary to previous heart surgery or atrial ablation procedures.
Electrocardiographically it is more difficult to classify since heart rate is more variable and “saw-tooth” waves are not clearly shown.
Atrial Flutter Treatment
Pharmacotherapy to revert flutter back to sinus rhythm is not very effective.
Furthermore, antiarrhythmic treatments class I can slow down atrial rates and therefore prompt 1:1 atrioventricular conduction, causing very high ventricular rates (200 bpm or higher) and clinical manifestations similar to those of ventricular tachycardia.
Ibutilide is the most efficient antiarrhythmic drug for the cardioversion of atrial flutter in 80% of cases, but there is up to a 4% risk of torsades de pointes and a 4.9% risk of monomorphic ventricular tachycardia, so it is necessary to monitor the patient during administration 4.
The most effective flutter treatment is electrical cardioversion, although it is usually used during acute episodes in patients with hemodynamic instability.
Options for acute, stable patients include heart rate control treatment with beta-blockers or verapamil.
The definitive typical flutter treatment is the cavotricuspid isthmus catheter ablation. This is a procedure that causes the interruption of the macro-reentry cycle, and has high success rates and few medical complications.
Atrial Flutter and Anticoagulation
Stroke risk associated to atrial flutter is slightly lower than that of atrial fibrillation.
However, chronic anticoagulation treatment is recommended following the same guidelines as with atrial fibrillation patients 1 2.
In our website we have a CHA2DS2-VASc score calculator available to help you assess the need for Anticoagulant treatment in patients with atrial flutter or atrial fibrillation.
After catheter ablation, anticoagulation treatment can be suspended after 4-6 weeks if the patient continues in sinus rhythm.