The P Wave
The P wave is one of several waves on the electrocardiogram (EKG). It is a small wave seen at the beginning of each cardiac cycle.
The P wave provides crucial information about atrial depolarization and heart rhythm disorders.
In this article, we will explore the complexities of the P wave, its importance and its implications in EKG analysis.
Normal P Wave
The P wave is the first deflection of the cardiac cycle seen on an EKG. It represents the electrical activity associated with atrial depolarization.
The normal P wave is a low amplitude, vertical, rounded wave, resembling a gentle hill, which is continued immediately from the QRS complex. Its normal duration is 0.08 s and 0.10 s (2 to 2.5 mm) in length, and a maximum amplitude of 0.25 mV (2.5 mm) in height 1.
As it is generated by the sinus node, the P wave is positive in all leads, except in lead aVR where it is negative and in lead V1 where it should be isobiphasic 1.
Components of the P wave
The P wave is formed by the superposition of the depolarization of the right atrium (initial part) and the left atrium (final part).
In lead V1, where the P wave is isobiphasic, it is common to observe both components, with the first positive portion corresponding to the right atrium and the second negative portion corresponding to the left atrium 1.
P Wave Disturbances
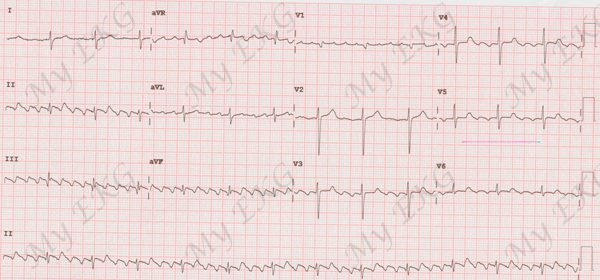
Right atrial enlargement
Related article: Right atrial enlargement.
Right atrial enlargement often results in P wave disturbances, especially in the initial part of the P wave.
Right atrial enlargement causes an increase in P wave amplitude, or in other words, a P wave higher than 2.5 mm. If it is not accompanied by left atrial enlargement there is no increase in P wave duration.
This high P wave with a normal duration is classically called P pulmonale. It is seen more clearly in inferior leads.
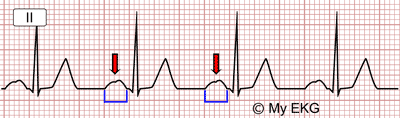
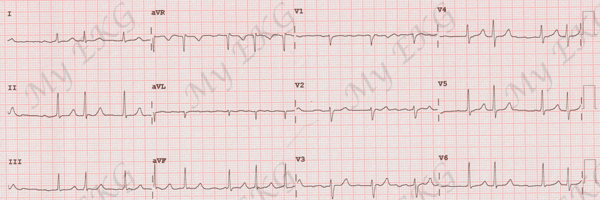
Right atrial enlargement:
P wave higher than 2.5 mV with normal duration.
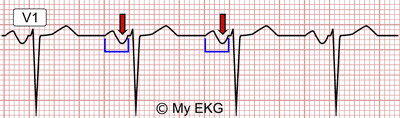
Right atrial enlargement:
P wave with its initial portion with higher voltage.
In lead V1, high initial component (greater than 1.5 mV) with normal duration is also observed.
To summarize: The most striking sign of right atrial enlargement is a high P wave, greater than 2.5 mm (2.5 mV) in inferior leads and with a high initial component in lead V1, greater than 1.5 mm.
The presence of pulmonary P wave in the electrocardiogram is a sign with limited sensitivity and specificity, since it is not always present when right atrial dilatation is detected by echocardiography, and can be observed in patients with normal right atrium 1.
More information: Right atrial enlargement.
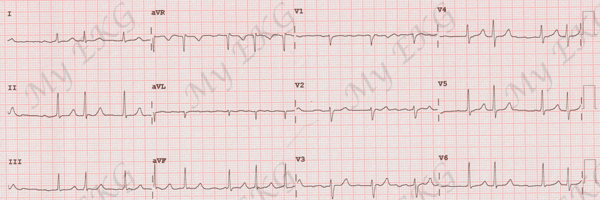
Left atrial enlargement
Related article: Left atrial enlargement.
In most cases, left atrial enlargement causes changes in the P wave, especially in its final component, with a widening of the P wave greater than 0.12 s being observed.
Occasionally, the right and left component of the P wave separate slightly giving the P wave a tiny "m" shape, classically called "mitral P wave".
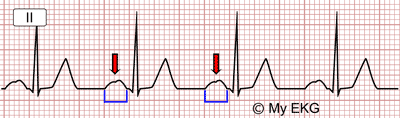
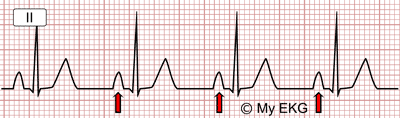
Left Atrial Enlargement
Wide P wave, greater than 0.12 s, P mitrale (red arrow).
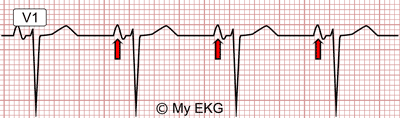
Left Atrial Enlargement:
Wide P wave with prominent negative component.
In addition, in lead V1 the depth of the negative final component is greater than the height of the initial part.
Summarizing: The most striking sign of the left atrial enlargement is a wide P wave, greater than 0.12 s or 3 small squares, with a predominance of the negative final component in lead V1.
The presence of electrocardiographic signs of left atrial enlargement is one of the criteria for the diagnosis of left ventricular hypertrophy, this is one of the few signs of LVH detectable on the EKG in patients with right bundle branch block (read left ventricular hypertrophy).
Ectopic P waves
Ectopic P waves are stimuli originating in a region of the atria different from the sinus node.
Ectopic P waves have a different morphology from normal P waves, being negative in the leads where the sinus P wave is usually positive (inferior, lateral or V2-V6 leads).
If the ectopic P waves are isolated, they are called atrial premature beats. If a rhythm occurs where all the P waves are ectopic, it is called, depending on the heart rate, ectopic atrial rhythm or atrial tachycardia.
Retrograde P waves
The retrograde P wave appears when an electrical stimulus from the AV junction or the ventricles depolarizes the atria. It is not a disturbance per se, but a consequence of another rhythm disturbance.
It usually appears in atrioventricular nodal reentrant tachycardia or ventricular arrhythmias, both in premature ventricular complexes and ventricular tachycardias.
It is usually observed as a negative wave in inferior leads. It is often inscribed within the QRS complex as a notch or as a false S wave in inferior leads that is not present in sinus rhythm.
It can also be observed in the ST-segment or inscribed above the T wave. In some cases it may be before the QRS complex as a negative P wave in the inferior leads with a short PR interval.
Absence of P Waves
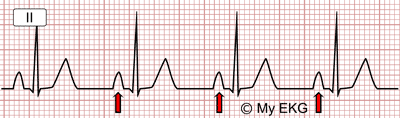
Atrial flutter
Related article: Atrial flutter.
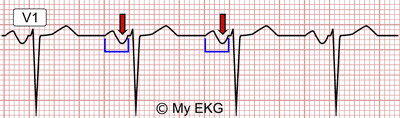
Typical counterclockwise atrial flutter:
Regular rhythm at 100 bpm with negative F waves in inferior leads.
In atrial flutter, P waves disappear, as normal atrial activity is replaced by a macroreentrant circuit in the atria with a very high frequency.
This activity causes "saw-tooth" waves, called F (flutter) waves, which are usually best seen in the inferior leads.
More information: Atrial flutter.
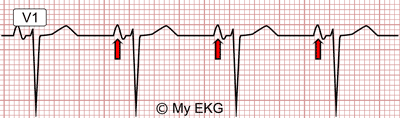
Atrial fibrillation
Related article: Atrial fibrillation.
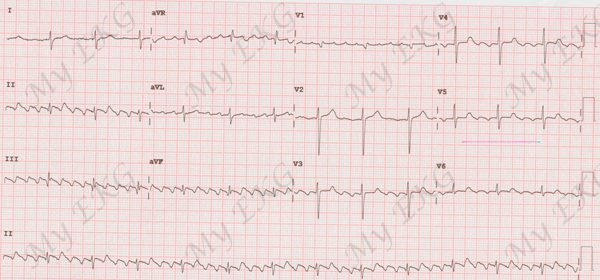
Atrial fibrillation:
Irregular rhythm at 66 bpm, absence of P waves, presence of small atrial waves with variable morphologies (f waves).
As there is chaotic atrial stimulation, in atrial fibrillation there are no P waves, although it is possible to observe small atrial waves with variable morphologies, called f waves (fibrillation).
The electrocardiogram of atrial fibrillation is characterized by completely irregular R-R intervals.
More information: Atrial fibrillation.
Escape rhythms
In the absence of sinus rhythm caused by sick sinus syndrome, an escape rhythm originating in the AV node or in the bundle of His often appears.
AV junctional rhythm (narrow QRS complexes) may also be observed in children and healthy athletes.
If escape rhythm occurs in the AV node, the escape rhythm will have narrow QRS complexes, unless accompanied by bundle branch block.
If the escape rhythm occurs below the bifurcation of the bundle of His, the QRS complexes will be wide.
The presence of complete AV block also causes an escape rhythm, although in this case the P waves are dissociated from the QRS complexes.
References
- 1. Surawicz B, Knilans TK. Chou’s electrocardiography in clinical practice, 6th ed. Philadelphia: Elservier; 2008.
- 2. Soos MP, McComb D. Sinus Arrhythmia. [Updated 2020 Jan 28]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK537011/.
- 3. Issa ZF, Miller JM, Zipes DP. Sinus Node Dysfunction. in Clinical Arrhythmology and Electrophysiology: A Companion to Braunwald's Heart Disease. Second Edition. W.B. Saunders; 2012, p. 164-174. doi: 10.1016/B978-1-4557-1274-8.00008-7.
If you Like it... Share it.