Supraventricular Tachycardias
Supraventricular tachycardia (SVT) are a group of tachycardias in which at least a structure above the bundle of His is necessary for its continuance.
Supraventricular tachycardias include a number of disorders, atrioventricular nodal reentrant tachycardia and atrioventricular reentry tachycardia being the most frequent. We also include in this article atrial tachycardia and Inappropriate sinus tachycardia, which are rare arrhythmias.
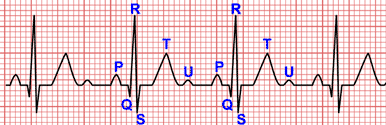
Supraventricular tachycardias are characterized on the EKG as regular tachycardias with narrow QRS complexes and high heart rate.
Although less frequent, wide QRS complexes can also turn up in SVT, as for example in AVRT with antidromic conduction, or if the SVT is accompanied by previous bundle branch block or aberrant conduction (Ashman phenomenon).
By concept, atrial fibrillation and atrial flutter are supraventricular tachycardias, but we prefer to study them individually in other articles.
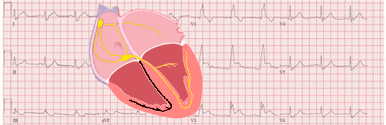
Atrioventricular Nodal Reentrant Tachycardia (AVNRT)
Related article: AV nodal reentrant tachycardia.
Atrioventricular nodal reentrant tachycardia is the most frequent of paroxysmal SVTs in healthy hearts, accounting for 60% of cases. It is usually exhibited by women in their forties.
It is caused by the presence of two pathways in the AV node — a slow and a fast one — that at the appearance of an extra stimulus form a reentry mechanism perpetuating tachycardia.
Atrioventricular nodal reentrant tachycardia
From an electrophysiological point of view there are two forms of atrioventricular nodal reentrant tachycardia: slow-fast AVNRT (Common AVNRT) and fast-slow AVNRT (Uncommon AVNRT).
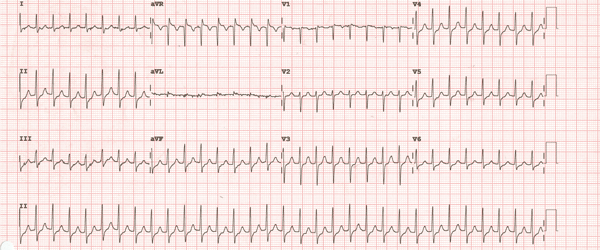
AVNRT characteristic findings on the electrocardiogram are:
- Regular narrow QRS complex tachycardia with heart rate between 120 and 250 bpm.
- Common AVNRT: absence of P waves (being embedded in the QRS), pseudo r’ waves in lead V1 or pseudo S waves in inferior leads.
- Uncommon AVNRT: negative P waves appears after the corresponding QRS (before T wave) in inferior leads.
As an AV node-related supraventricular tachycardia, it is usually stopped by the undertaking of vagal manoeuvres or the use of intravenously administered adenosine.
We would like to remind you that the use of intravenous adenosine must be administered by experienced medical staff and require patient monitoring.
Atrioventricular nodal reentrant tachycardia definitive treatment is slow pathway catheter ablation.
More information: AV nodal reentrant tachycardia.
Atrioventricular Reentry Tachycardia (AVRT)
Up to a third of the patients diagnosed with pre-excitation syndrome by electrocardiogram can present SVTs related to accessory pathways 1.
These tachycardias are produced by a mechanism of macro-reentry, involving the atria, the conduction system, the ventricles and the accessory pathway. The electrical stimulus is conducted continuously through all these parts perpetuating tachycardia.
There are two very different electrocardiographic patterns based on the direction of the stimulus conduction:
Orthodromic Tachycardia:
The stimulus is conducted from the atria to the ventricles by the conduction system returns to the atria by the accessory pathway. As the ventricles are stimulated by the conduction system, the QRS complex is narrow.
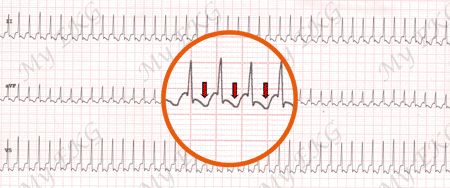
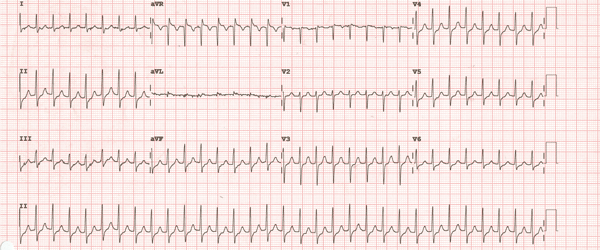
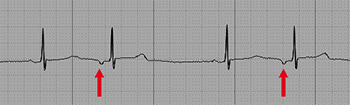
Orthodromic tachycardia at 250 bpm
Narrow QRS complex tachycardia. P waves after the QRS in red.
Electrocardiogram features of orthodromic tachycardia:
- Narrow QRS complex tachycardia with HR between 200 and 300 bpm.
- Non-sinus P waves can be found following the QRS complex.
Antidromic Tachycardia:
The stimulus is conducted from the atria to the ventricles via the accessory pathway, and returns to the atria via the conduction system. As the ventricular depolarisation occurs completely by the accessory pathway, the QRS complex is wide.
Antidromic tachycardia is a supraventricular tachycardia with wide QRS complexes.
Electrocardiogram features of antidromic tachycardia:
Atrial Tachycardia
Atrial tachycardia is a rare supraventricular tachycardia. As suggested by its name, it originates in the atrial muscle and does not require the atrioventricular node or the ventricles for its initiation and continuance.
During an atrial tachycardia the AV node can present blocks of varying degrees depending on the conduction capacity of the atrioventricular node, with the possibility of AV conduction ratio of 1:1, 2:1, etc.
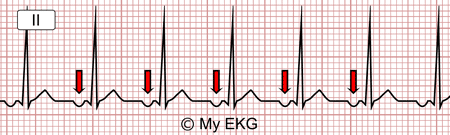
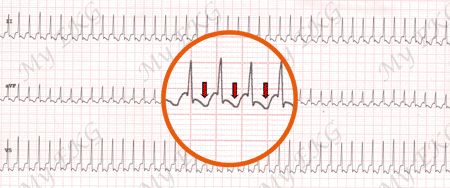
Atrial tachycardia:
Tachycardia at 125 bpm with ectopic P waves (negative P wave in lead II)
Atrial tachycardia characteristic findings on the electrocardiogram:
- Well defined P waves with rates from 100 to 240 bpm.
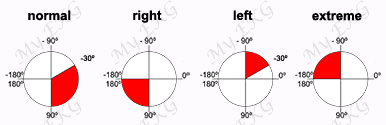
- P wave has a different morphology and electrical axis than sinus P wave.
- P waves are usually closer to the following QRS complex than to the preceding one (PR interval shorter than RP interval).
- Narrow QRS complex, unless preexisting bundle branch block or aberrant conduction
With very high heart rates it is difficult for P waves to be distinguished, making it impossible to differentiate atrial tachycardia from other supraventricular tachycardia.
Vagal manoeuvres or intravenous Adenosine administration can produce a transitory AV block, allowing hidden P waves to be seen.
Unlike supraventricular tachycardia in which the AV node is involved, adenosine does not usually interrupt the arrhythmia in atrial tachycardia.
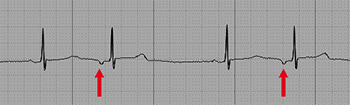
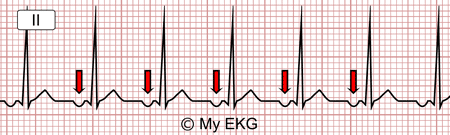
Atrial Extrasystoles
Atrial extrasystoles are premature electrical impulses generated in an atrial area other than the sinus node.
Characteristic findings on EKG are the occurrence of isolated P waves with different morphology and electrical axis than in sinus rhythm, followed by a QRS complex similar to previous ones.
Atrial extrasystoles
As in ventricular extrasystoles, the ectopic P wave often arises prematurely (shorter P-P interval as compared to previous ones).
In atrial extrasystoles the PR interval can be normal or shortened.
Atrioventricular conduction may be normal or blocked if atrial extrasystole occurs during the refractory period of the AV node.
It may be difficult to identify the atrial extrasystole P wave on some electrocardiograms, as it may be hidden in the preceding QRS or T wave.
Atrial extrasystoles do not require treatment unless secondary to other pathology or very symptomatic.
Inappropriate Sinus Tachycardia
Related article: Inappropriate sinus tachycardia.
Inappropriate sinus tachycardia is a rare supraventricular tachycardia caused by a increase at sinus node level in heart rate at minimal exercise or at rest.
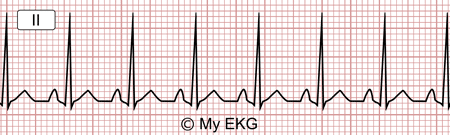
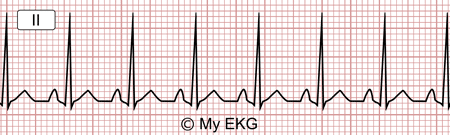
Sinus tachycardia at 136 bpm
Inappropriate sinus tachycardia electrocardiogram features are the same as sinus tachycardia.
It is more common in young women and is usually very symptomatic. Its diagnosis is made after ruling out other supraventricular tachycardias and other causes of sinus tachycardia.
More information: Inappropriate sinus tachycardia.
Supraventricular Tachycardia Summary
Supraventricular tachycardiad are a group of heart rhythm disorders which cause rhythmic narrow QRS complex tachycardias in most cases.
By concept, for their maintenance, SVTs need at least one structure above the bundle of His.
They usually have a benign prognosis, although they are usually very symptomatic and with frequent recurrences.
Although medical treatment with antiarrhythmic drugs is usually effective, catheter ablation is the treatment of choice as a definitive, high success rate solution.
We hope we have been helpful in expanding your knowledge of supraventricular tachycardias.
References
- 1. Almendral J, Castellanos E, Ortiz M. Paroxysmal Supraventricular Tachycardias and Preexcitation Syndromes. Rev Esp Cardiol. 2012;65(5):456-69. doi: 10.1016/j.rec.2011.11.020
- 2. Surawicz B, Knilans TK. Chou’s electrocardiography in clinical practice, 6th ed. Philadelphia: Elservier; 2008.
- 3. Katritsis DG, Camm AJ. Katritsis DG, Camm AJ. Atrioventricular Nodal Reentrant Tachycardia. Circulation. 2010;122:831-840. doi: 10.1161/CIRCULATIONAHA.110.936591
If you Like it... Share it.