Atypical Presentations of STEMI on the EKG
Acute occlusion of a coronary artery usually causes an elevation of the ST segment on the electrocardiogram.
The changes in the EKG accompanied by the clinical picture help diagnose ST-segment elevation myocardial infarction (STEMI), and allows urgent measures to be taken for coronary reperfusion.
But, in some patients, the occlusion of a coronary artery does not produce elevation of the ST-segment in the EKG or the STEMI is difficult to diagnose, leading to a delay in treatment, a greater extension of the infarction and a worse evolution.
The following disorders may delay the diagnosis of an acute myocardial infarction either by making it difficult to diagnose (left bundle branch block, pacemaker pacing), or by features on the electrocardiogram other than ST elevation (posterior myocardial infarction, left main coronary artery occlusion).
Although no ST-segment elevation is found in the standard EKG, if coronary occlusion is suspected, they will be diagnosed with STEMI and should receive urgent treatment.
Left Bundle Branch Block
Related article: Modified Sgarbossa criteria.
Acute Myocardial Infarction Debuting with Left Bundle Branch Block
Acute myocardial infarction may cause conduction disturbances such as AV blocks, left fascicular blocks or bundle branch blocks.
Of all the conduction disorders, the left bundle branch block is the only one that "hides" the ST-segment elevation of the acute myocardial infarction due to its own repolarization disturbances.
According to the ESC Guidelines for the Management of STEMI 1: The presence of concordant ST-segment elevation appears to be one of the best indicators of ongoing myocardial infarction with an occluded infarct artery
Patients with a clinical suspicion of ongoing myocardial ischaemia and left bundle branch block should be managed in a way similar to STEMI patients, regardless of whether the left bundle branch block is previously known.
It is important to remark that the presence of a (presumed) new left bundle branch block does not predict an myocardial infarction per se 1.
The modified Sgarbossa criteria may be useful in these cases to diagnose acute myocardial infarction with left bundle branch block.
In these patients, medical questioning and the associated clinical picture are important, because most patients with chest pain and left bundle branch block on the EKG do not present an acute myocardial infarction.
Acute Myocardial Infarction in Patients with Previous Left Bundle Branch Block
Previous left bundle branch block also makes it difficult to diagnose ST-segment abnormalities of acute myocardial infarction.
There are several electrocardiographic signs to try to diagnose a STEMI with left bundle branch block. The most significant sign is the elevation of the ST-segment in predominantly positive leads (in left bundle branch block, the ST-segment and the T wave are usually opposite to the QRS complex).
In these cases, the modified Sgarbossa criteria may also be useful for the diagnosis of an acute myocardial infarction.
Urgent reperfusion therapy is also recommended in patients with a clinical picture suggestive of STEMI and previously known left bundle branch block.
More information: Modified Sgarbossa criteria.
Acute Myocardial Infarction and Ventricular Pacing
Ventricular pacing may also prevents a correct evaluation of an electrocardiogram in a patient with suspected acute myocardial infarction.
Ventricular pacing usually generates QRS complexes similar to left bundle branch block, with the same difficulties described above.
In the case of suspicion of STEMI, it is recommended, in patients who are not dependent on ventricular pacing, to reprogram the pacemaker and perform an electrocardiogram with the intrinsic heart rhythm.
If this is not possible (ventricular pacing dependency patients or if a programmer is not available), the possibility of urgent coronary angiography should be evaluated.
In the diagnosis of myocardial ischemia during ventricular pacing, the Sgarbossa criteria may also be applied although they are less specific.
Isolated Posterior Myocardial Infarction
Acute posterior myocardial infarction, which normally is caused by the occlusion of the circumflex artery, does not cause ST-segment elevation on a standard electrocardiogram.
Its main sign on the EKG is a depression of the ST-segment greater than 0.5 mm in the leads from V1 to V3. If the final component of the T wave is positive, it increases the diagnostic suspicion 1 2.
The presence of tall R waves in these leads also favors the diagnosis of posterior myocardial infarction.
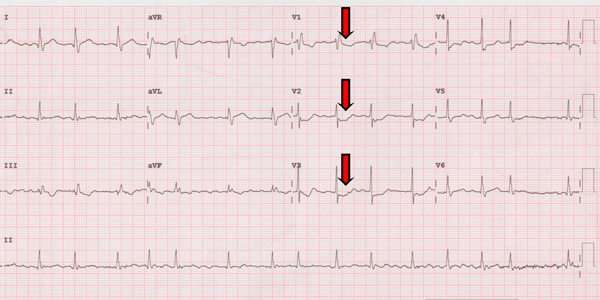
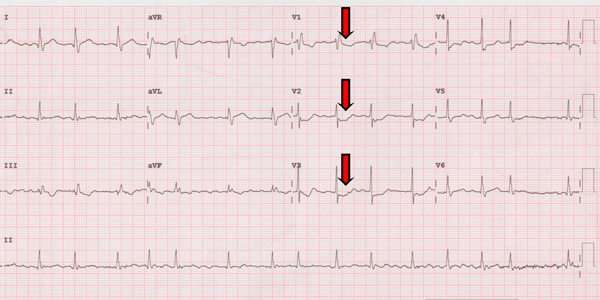
Electrocardiogram of a posterior myocardial infarction:
ST-segment depression and prominent R wave in leads V1 to V3.
An electrocardiogram with posterior leads should be performed to confirm the diagnosis, observing an ST-segment elevation greater than 0.5 mm in leads V7 to V9 1.
Posterior myocardial infarction is an ST-segment elevation myocardial infarction and should be treated as such.
Left Main Disease. Widespread ST Depression
The total or subtotal occlusion of the left main coronary artery is one of the most severe acute coronary syndromes, since it produces the interruption of the flow in the left anterior descending artery and in the circumflex artery, suffering ischemia in a large region of the heart. Without urgent reperfusion therapy it is usually fatal.
It usually leads to hemodynamic instability, heart failure and ventricular arrhythmias.
On the EKG, left main disease is observed as ST-segment depression greater than 0.1 mV (1 mm) in 8 or more leads coupled with ST-segment elevation in lead aVR and/or in lead V1 2 3.
If left main disease is suspected on the electrocardiogram, an urgent coronary angiography and reperfusion therapy should be performed.
In patients with disease in several coronary arteries (elderly patients with several risk factors) a similar electrocardiogram may be observed.
Summary
Certain disorders may cause an occlusion of a coronary artery not to be diagnosed as STEMI, causing a delay in the reperfusion therapy and increasing the risk of complications and death.
We must be guided by the clinical picture and the described EKG changes to avoid overlooking an acute myocardial infarction.
Finally, a major clinical suspicion of occlusion of a coronary artery that does not respond to medical treatment is a criterion for urgent coronary angiography even in the absence of ST-segment elevation.
References
- 1. Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the Management of Acute Myocardial Infarction in Patients Presenting With ST-Segment Elevation: The Task Force for the Management of Acute Myocardial Infarction in Patients Presenting With ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J 2017; Aug 26. doi 10.1093/eurheartj/ehx393.
- 2. O'Gara PT, Kushner FG, et al. 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:e362–e425. doi CIR.0b013e3182742cf6.
- 3. Wagner GS, Macfarlane P, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part VI: acute ischemia/infarction. J Am Coll Cardiol. 2009 Mar 17;53(11):1003-11. doi: 10.1016/j.jacc.2008.12.016.
If you Like it... Share it..