Ventricular Arrhythmias
Ventricular arrhythmias are a group of rhythm disorders which arise distal to the bundle of His 1.
As ventricular stimuli are not conducted by the intraventricular conduction system, its QRS complex is wide due to a mechanism similar to bundle branch blocks.
The most common cause of ventricular arrhythmias is the onset of ectopic stimuli (ventricular extrasystoles, ventricular tachycardia), but they also might be originated as an escape phenomenon in the absence of atrial stimuli.
The electrocardiogram is a key test in ventricular arrhythmias, especially in the most serious cases such as ventricular tachycardia.
Whenever the stability of the patient allows it, we must have a 12-lead EKG and a rhythm strip performed in order to diagnose the type of arrhythmia and whether it is ventricular or supraventricular tachycardia.
Premature Ventricular Complexes
Related article: Premature ventricular complexes.
Isolated premature ventricular complex:
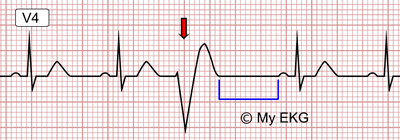
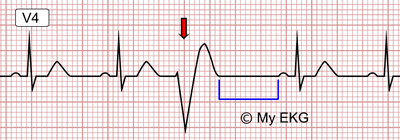
PVC marked by the arrow on an EKG in sinus rhythm. The compensatory pause is marked in blue.
Premature ventricular complexes (PVCs) are ectopic stimuli originated in the ventricles which cause a premature ventricular depolarization 2.
PVCs occur in patients with or without structural heart disease and tend to become more prevalent with increasing age. They can increase in number in clinical situations such as infections, ischemia, stress or consumption of toxic substances.
Premature Ventricular Complexes on the Electrocardiogram
- Premature QRS complex in relation to the expected impulse of the basic rhythm.
- Abnormal QRS complex in duration and morphology. It is accompanied by ST-segment and T wave changes.
- The premature ventricular complex is not preceded by a P wave.
- Full compensatory pause: after the PVCs a delay occurs until the appearance of basic rhythm.
Premature Ventricular Complexes Classification
According Number of Foci:
- Unifocal: every premature ventricular complex presents the same morphology.
- Multifocal: presence of PVCs with different morphologies.
According to Frequency
- Frequent: 10 or more PVCs per hour, or 6 PVCs or more per minute.
- Occasional: fewer than 10 PVCs per hour, or fewer than 5 per minute.
According to Pattern of Presentation:
- Isolated PVC: there is no regular repeating pattern.
- Ventricular bigeminy: every sinus beat is followed by a premature ventricular complex.
- Ventricular trigeminy: every second sinus beat is followed by a PVC.
- Ventricular quadrigeminy: every third sinus beat is followed by a PVC.
- Couplet: two consecutive PVCs.
- Nonsustained ventricular tachycardia: three or more consecutive PVCs.

Ventricular bigeminy: premature ventricular complexes alternating with a normal beat.
Three or more consecutive PVCs are by definition a ventricular tachycardia.
Patients with atrial fibrillation may have isolated beats with wide QRS due to aberrant ventricular conduction (Ashman phenomenon), which may cause diagnostic confusion with premature ventricular complexes.
The diagnosis of these phenomenon is mainly based on the presence of the long-short sequence that ended in a wide QRS complex without compensatory pause (read Ashman phenomenon).
More information: Premature ventricular complexes.
Ventricular Escape Rhythm or Idioventricular Rhythm
Ventricular escape rhythm or idioventricular rhythm occurs in the absence of supraventricular stimuli or with bradycardias with heart rate below 40 bpm (sick sinus syndrome or complete AV block distal to the bundle of His) 3.
Ventricular escape rhythm is observed on the electrocardiogram as a slow, regular rhythm (between 20 and 50 bpm) with broad QRS complexes.
Sometimes it is impossible to tell a ventricular escape rhythm apart from a junctional escape rhythm with associated bundle branch block.
Normally no P waves are seen, but disassociated P waves or retrograde P waves could be seen less often.
Accelerated Idioventricular Rhythm
Accelerated idioventricular rhythm (AIVR) is mainly observed after the reperfusion of an occluded artery in an acute coronary syndrome and is caused by an abnormal automatism of the ventricles.
The electrocardiogram shows a rhythm with QRS complexes that have ventricular morphology (similar to ventricular tachycardia) but with low rates (between 60 and 110 bpm) and gradual onset and termination that set it apart from ventricular tachycardia, which usually starts with a premature ventricular complex.
It is a sign of coronary reperfusion, so its appearance in a ST-segment elevation myocardial infarction indicates a good prognosis.
Ventricular Tachycardia
Related articles: Ventricular tachycardias, ventricular tachycardia criteria.
We speak of ventricular tachycardia (VT) when there are three or more consecutive ventricular beats. If their duration is less than 30 seconds it is called non-sustained ventricular tachycardia; if it is longer than 30 seconds or an electrical cardioversion is needed, it is called sustained ventricular tachycardia.
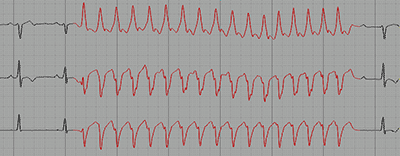
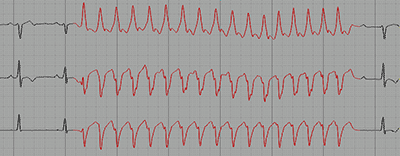
Non-sustained monomorphic ventricular tachycardia, 17 beats.
The main cause of of ventricular tachycardia is coronary artery disease due to re-entry mechanisms in regions damaged by a previous infarction.
Other causes include dilated or hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy, valvular disease, sarcoidosis and Chagas disease among others.
Ventricular tachycardias are usually regular, with heart rates between 100 and 250 bpm, but it can show an irregular rhythm in certain cases.
In VT atrial activity is independent of the ventricles, unless a ventriculoatrial conduction is present.
Remember: all wide QRS complex tachycardia is a ventricular tachycardia until proven otherwise.
Its clinical manifestations vary from few symptoms or palpitations to cardiac arrest, and also include syncope, heart failure and cardiogenic shock.
When all QRS complexes in the VT have the same morphology it is called monomorphic ventricular tachycardia. On the contrary, when the morphology of the QRS complexes differ from each other it is called polymorphic ventricular tachycardia.
Torsades de Pointes
Related article: Torsades de pointes.
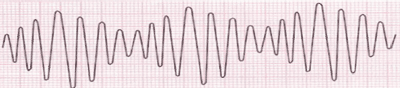
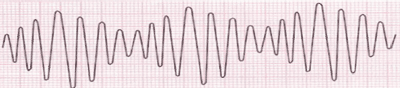
Electrocardiogram of torsades de pointes.
Torsades de pointes is a type of polymorphic VT associated with the presence of prolonged QT interval.
On the EKG it is characterized by QRS complexes varying in amplitude which seem to rotate around the isoelectric line.
More information: Ventricular tachycardias, ventricular tachycardia criteria, torsades de pointes.
Ventricular Fibrillation
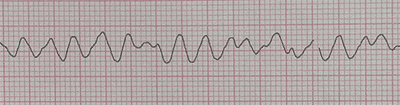
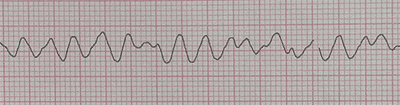
Electrocardiogram with ventricular fibrillation.
Ventricular fibrillation is a fast, irregular ventricular rhythm (higher than 250 beats per minute) with chaotic morphology that leads to the absolute loss of cardiac contraction. It is mortal if left untreated.
Its main cause is coronary artery disease, although it may occur in most heart diseases. These include hypertrophic and dilated cardiomyopathy. The only effective treatment is electrical defibrillation.
Ventricular fibrillation main characteristic on the EKG is the undulations which are irregular both in shape and morphology, with no clearly identifiable QRS complexes or T waves.
Remember: ventricular fibrillation is a cardiac arrest and its only effective treatment is electrical defibrillation.
References
- 1. Surawicz B, Knilans TK. Chou’s electrocardiography in clinical practice, 6th ed. Philadelphia: Elservier; 2008.
- 2. Goldberger A, Goldberger Z, Schvilkin A. Clinical Electrocardiography: A Simplified Approach, 7th ed. Philadelphia: Mosby Elservier; 2006.
- 3. Uribe W, Duque M, Medina E. Electrocardiografía y Arritmias. Bogotá: P.L.A. Export Editores Ltda; 2005.
If you Like it... Share it.