Ventricular Septal Defects (VSD) on the Electrocardiogram
Authors: Eduardo Consuegra Llapur, Ernesto C. Amalfi Aguilera.
The International Society for Nomenclature of Paediatric and Congenital Heart Disease (ISNPCHD) has defined a ventricular septal defect (VSD) as a congenital cardiac malformation in which there is a hole or pathway between the ventricular chambers 1.
Ventricular septal defect is the most common congenital heart disease if the bicuspid aortic valve is excluded 2.
This defect may be single or multiple and of varying size and shape.
It may also be associated with other cardiac anomalies such as tetralogy of Fallot, persistent truncus arteriosus, transposition of the great vessels or the common atrioventricular canal, or may also occur in isolation.
Classification of Ventricular Septal Defects
Ventricular septal defects are classified depending on the site of the ventricular septum where the defect is present 3:
- Perimembranous central VSD
- Inlet VSD without a common AV junction
- Trabecular muscular VSD
- Outlet VSD
Perimembranous Central VSD
Perimembranous central defects are the most frequent VSD, between 75% and 80% of them.
They are located in the space usually occupied by the interventricular part of the membranous septum, at the anteroseptal commissure behind the septal leaflet of the tricuspid valve and below the commissure between the right and noncoronary leaflets of the aortic valve 3.
Inlet VSD without a Common AV Junction
Inlet defects represent 5% to 8% of all VSD. They open into the right ventricle inlet and extend along the septal leaflet of the tricuspid valve.
They are located below the medial papillary muscle, postero-inferior limb of the septal band, and anteroseptal commissure of the tricuspid valve.
Trabecular Muscular VSD
Between 5% and 20% of all ventricular septal defects are trabecular muscular defects. Many trabecular muscular defects close spontaneously without intervention.
Trabecular muscular defects are located within the apical muscular component of the ventricular septum. Some are complex, with multiple entrances and exits on both sides of the ventricular septum (“Swiss cheese defects”) 3.
Outlet VSD
Outlet defects represent 5% to 7% of all VSD, although this incidence is increasing in the Asian population where it can reach 30%.
Outlet defects open into the right ventricle outlet between the limbs of the septal band, just below the pulmonary valve 3.
Causes of EKG Disorders
The extra blood supply to the right ventricle from the left ventricle causes increased lung flow, which results in left atrial enlargement and left ventricular hypertrophy.
The electrocardiogram varies depending on the impact of the defect. It may be normal in small defects or show signs of left atrial and left ventricular enlargement according to the magnitude of the shunt due to volume overload of these chambers.
As pulmonary resistances increase in response to pulmonary hyper-flow, the right ventricle will also develops hypertrophy.
Electrocardiogram in Ventricular Septal Defect
In this article we will only describe changes in the EKG when the VSD is not associated with other cardiac malformation.
Small septal defects with a small left-right shunt are almost always accompanied by normal EKG 5.
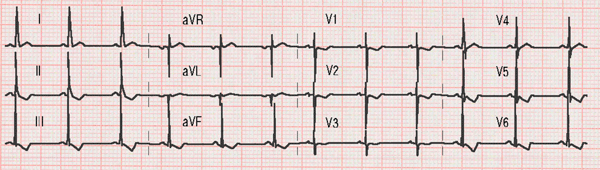
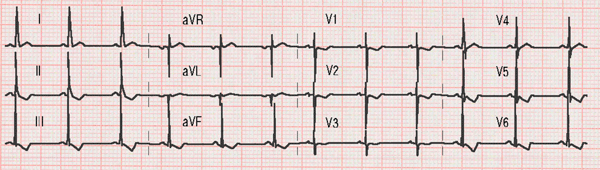
Ventricular septal defect:
Slight widening of the P waves in lead II (left atrial enlargement), deep S waves in lead V1 and tall R waves in leads V5 and V6 (left ventricular hypertrophy).
Left atrial enlargement and left ventricular hypertrophy are usually the most frequent alteration, this is due to the overloading of left chambers due to pulmonary overcirculation 4.
Wide P waves caused by left atrial growth are usually observed on the EKG. In addition, signs of left ventricular hypertrophy appear with deep S waves in lead V1 and tall R waves in the left precordial leads (V5 and V6) 6.
Moderate or severe defects may cause right ventricular hypertrophy, especially if there is an increase in pressure in the right ventricle.
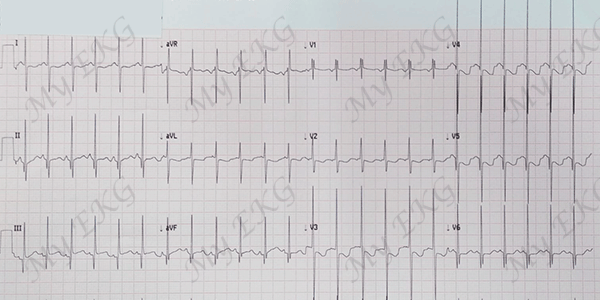
Two-month-old patient with severe ventricular septal defect:
Signs of left ventricular hypertrophy with deep S waves in lead V1 and tall R waves in leads V5 and V6. Tall R waves in leads V1-V3 and deep S waves in leads V5 and V6 with negative T waves in leads V2 to V5 (juvenile T wave pattern) are secondary to the age-specific predominance of the right ventricle.
Patients with a severe interventricular septal defect often have electrocardiographic signs of biventricular hypertrophy, with high QRS and diphasic complexes in the midprecordial leads (V2, V3 and V4), alterations also known as Katz-Wachtel phenomenon or sign.
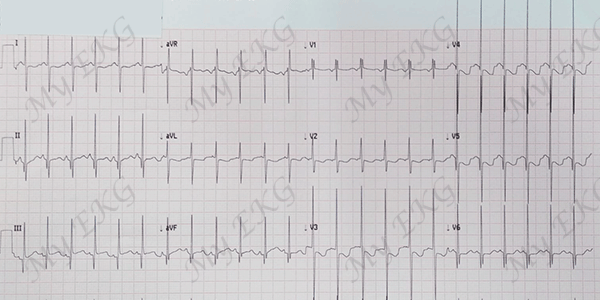
Katz Wachtel phenomenon:
The presence of biphasic QRS complexes with high amplitudes (≥50 mm) in the midprecordial leads (from V2 to V3 or to V4) is highly suggestive of biventricular hypertrophy and is characteristic of ventricular septal defect 6.
References
- 1. Franklin RC, Béland MJ et al. Nomenclature for congenital and paediatric cardiac disease: the International Paediatric and Congenital Cardiac Code (IPCCC) and the Eleventh Iteration of the International Classification of Diseases (ICD-11). Cardiol Young. 2017; 27: 1872-1938. doi: 10.1017/S1047951117002244.
- 2. Allen HD, Gutgesell HP, Clark EB, Dricoll DJ: Moss and Adam’s Heart Disease and Infants, Children and Adolescents Incluiding the Fetus and Young Adult, 6th ed. Philadelphia, PA, Lippincott Williams & Wilkins, 2001.
- 3. Lopez L, Houyel L, et al. Classification of Ventricular Septal Defects for the Eleventh Iteration of the International Classification of Diseases—Striving for Consensus: A Report From the International Society for Nomenclature of Paediatric and Congenital Heart Disease. Ann Thorac Surg 2018; 106:1578–89. doi: 10.1016/j.athoracsur.2018.06.020.
- 4. Moller J, Neal WA. Fetal, Neonatal And Infant Cardiac Disease. Mcgraw- Hill/Appleton & Lange, 1992.
- 5. Surawicz B, Knilans TK. Chou’s electrocardiography in clinical practice, 6th ed. Philadelphia: Elservier; 2008.
- 6. Rijnbeek PR, Witsenburg M, Schrama E, et al. New normal limits for the paediatric electrocardiogram. Eur Heart J. 2001; 22(8):702-11. doi: 10.1053/euhj.2000.2399.
- 7. Katz LN and Wachtel H. The diphasic QRS type of electrocardiogram in congenital heart disease. Am Heart J. 1937; 13: 202-206. doi: 10.1016/S0002-8703(37)91211-0.
If you Like it... Share it.