Pulmonary Stenosis on the Electrocardiogram
Authors: Eduardo Consuegra Llapur, Ernesto C. Amalfi Aguilera.
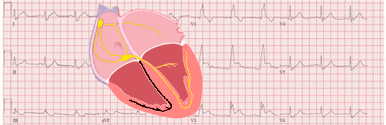
Pulmonary stenosis is a condition characterized by obstruction to blood flow from the right ventricle to the pulmonary artery.
The obstruction to the right ventricle outflow tract may be the result of abnormalities at the infundibulum, the pulmonary valve, the supravalvular region, or the branch and/or peripheral pulmonary arteries.
The EKG is an excellent tool for evaluating the severity of pulmonary stenosis. Electrocardiographic changes of right atrial enlargement and right ventricle hypertrophy may be observed in severe pulmonary stenosis.
The pulmonary stenosis can be classified into three groups depending on the location of the obstruction: supravalvular, valvular, and subvalvular stenosis 1 2.
Supravalvar Stenosis
Supravalvar stenosis, also known as pulmonary arterial stenosis or peripheral pulmonary stenosis, is caused by narrowing of the main pulmonary trunk, pulmonary arterial bifurcation, or pulmonary branches 2 4.
Supravalvar stenosis seldom occurs in isolation, and may occur in tetralogy of Fallot, Williams–Beuren syndrome, Noonan syndrome, Keutel syndrome, congenital rubella syndrome, or Alagille syndrome 4. It may also be associated with tetralogy of Fallot 4.
Valvar Stenosis
Valvar stenosis is usually an isolated lesion, it is the most common type of right ventricular outflow tract obstruction (80-90%), and constitutes 7.5% to 12.0% of all congenital heart diseases 1 4.
It results from thickening and fusion of the leaflets of the pulmonary valve, leading to a decrease in the opening area.
Valvar stenosis may be associated with Noonan syndrome, in which 60% have a dysplastic valve 2, and congenital rubella. It also may be associated with other congenital heart disease, such as tetralogy of Fallot, double outlet right ventricle, univentricular atrioventricular connection, and atrioventricular canal defect 3.
Subvalvar Stenosis
Subvalvar stenosis, also known as infundibular pulmonary stenosis, is an uncommon condition and it is caused by primary fibromuscular narrowing below the pulmonary valve, or right ventricular hypertrophy 2 3.
At the infundibular level, and to some extent the subinfundibular level, the obstruction tends to be dynamic, meaning that the orifice narrows during systole 4.
It is often associated with other congenital cardiac conditions including tetralogy of Fallot, ventricular septal defect or double-chambered right ventricle.
Clinical Presentation of Pulmonary Stenosis
Mild and moderate pulmonary stenosis are well tolerated, although, patients with moderate pulmonary stenosis may begin to have symptoms of dyspnea on exertion 2.
Severe pulmonary stenosis leads to right ventricular failure, and these patients complain of dyspnea, lower extremity swelling, and abdominal fullness. It may also lead to exertional symptoms of dyspnea, angina, and syncope 2.
The physical examination in severe pulmonary stenosis shows a systolic ejection murmur heard best over the left upper sternal border, and a prominent jugular venous a wave.
There may also be liver congestion, edema, and ascites 2. If the right atrial (RA) pressure increases, the opening of a patent foramen ovale may occur along with cyanosis 5.
Electrocardiogram of the Pulmonary Stenosis
As the pulmonary stenosis progresses to the severe form, the right ventricular wall stress increases leading to right ventricle hypertrophy 2.
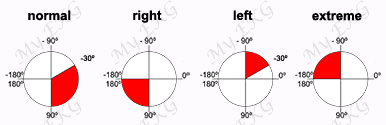
The EKG is an excellent tool for evaluating the severity of pulmonary stenosis. In mild pulmonary stenosis the EKG may be normal or show mild right axis deviation in the frontal plane 6.
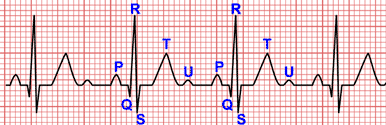
In moderate pulmonary stenosis the R wave amplitude in lead V1 exceeds the normal limits, and occasionally an rsR’ pattern may be present.
In severe pulmonary stenosis, right axis deviation is marked and associated with a monophasic R wave in lead V1, usually of >20 mm amplitude.
Right atrial enlargement evidenced by peaked and tall P waves in leads II and V1 is also commonly. With very severe obstruction, Q waves are present in the right precordial leads.
In children and adolescents with isolated pulmonary stenosis, there is good correlation between the height of the R wave in lead V1 and the right ventricular systolic pressure. The height of the R wave multiplied by 5 estimates the right ventricular systolic pressure in mmHg 6.
References
- 1. Rao PS. Management of Congenital Heart Disease: State of the Art; Part I—ACYANOTIC Heart Defects. Children (Basel). 2019 Mar; 6(3): 42. doi:
10.3390/children6030042.
- 2. Fitzgerald KP, Lim MJ. The Pulmonary Valve. Cardiology Clinics. 2011; 29(2), 223–227. doi: 10.1016/j.ccl.2011.01.006.
- 3. Waller BF, Howard J, Fess S. Pathology of pulmonic valve stenosis and pure regurgitation. Clinical Cardiology. 1995; 18(1), 45–50.
doi: 10.1002/clc.4960180112.
- 4. Baumgartner H, Bonhoeffer P, De Groot NMS. ESC Guidelines for the management of grown-up congenital heart disease (new version 2010). European Heart Journal. 2010; 31, 2915–2957. doi: 10.1093/eurheartj/ehq249
- 5. Bashore TM. Adult Congenital Heart Disease. Right Ventricular Outflow Tract Lesions. Circulation. 2007;115:1933–1947. doi: 10.1161/CIRCULATIONAHA.105.592345
- 6. Surawicz B, Knilans TK. Chou’s electrocardiography in clinical practice, 6th ed. Philadelphia: Elservier; 2008.
If you Like it... Share it.