Wellens Syndrome
Wellens syndrome was first described by Zwann and Wellens 1 in 1982 when they found a correlation between a precise EKG pattern in patients with unstable angina and the critical stenosis of the left anterior descending artery.
This syndrome is characterised by T wave abnormalities in the anterior chest leads associated with a critical stenosis of the proximal left anterior descending artery and carries an immediately life-threatening prognosis if not recognized promptly 2 3.
This EKG pattern is highly specific for an imminent anterior wall myocardial infarction as up to 75% of these patients develop extensive infarction of the anterior wall if left untreated 1.
Wellens syndrome is also called left anterior descending artery syndrome.
Clinical Presentation of Wellens Syndrome
Patients with Wellens syndrome are associated with previous angina, although, on presentation to the emergency department, patients will usually be pain-free. However, the T wave abnormalities on the EKG may persist 4.
The majority of these patients usually have negative or slightly increased cardiac biomarkers 2 4 5.
Electrocardiogram of Wellens Syndrome
The EKG shall be the only indication of an imminent massive anterior infarction 2.
Wellens syndrome has two EKG patterns:
- Type A shows biphasic T wave in precordial leads V2 and V3.
- Type B is characterized by deep negative symmetric T waves from leads V1 to V4.
It is also common to find absence of ST-segment elevation, preservation of precordial R wave progression and no precordial Q wave.
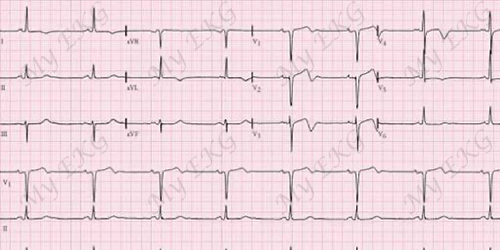
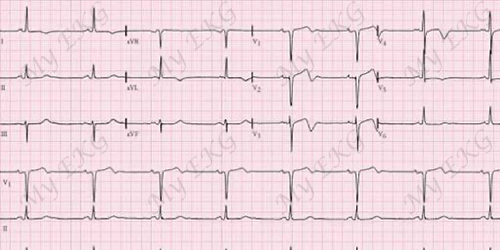
Electrocardiogram of Wellens syndrome type A:
Biphasic T wave in precordial leads V2 and V3.
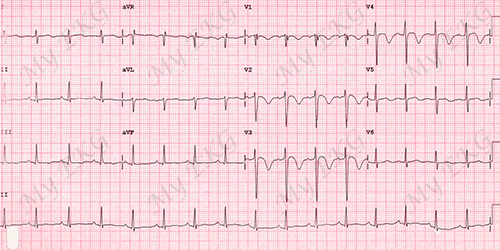
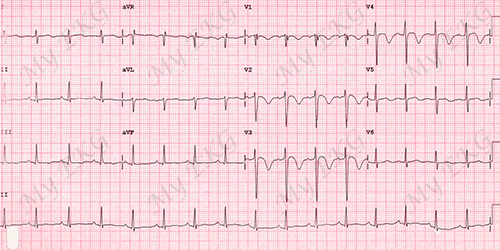
Electrocardiogram of Wellens syndrome type B:
Deep negative symmetric T waves from V1 to V4.
The T wave abnormalities are persistent and may remain in place for hours to weeks, and it is even possible to find these changes in symptoms-free patients 6.
In symptomatic patients, T wave abnormalities can normalise or evolve into ST-segment elevation 2.
It is vital that the physician recognize these changes and their association with critical left anterior descending artery obstruction and significant risk for anterior wall myocardial infarction 6.
Diagnosis of Wellens syndrome
Proposed criteria for the diagnosis of Wellens syndrome include all of the following 1 5 6:
- Characteristic T waves patterns, either type A (biphasic T waves in leads V2 and V3), or type B (deep and symmetrical T wave inversion from V1 to V4).
- No significant ST-segment elevation, with normal R wave progression in precordial leads.
- History of anginal chest pain.
- Normal or minimally elevated cardiac enzyme levels.
Stress tests are not recommended due to the possibility of progression to complete occlusion 5.
Now in the era of advanced imaging, it is possible to confirm he diagnosis in hemodynamically stable patients using non-invasive coronary CT angiogram before proceeding to definitive management using invasive catheter angiography 5.
Visualization of coronary vasculature with coronary CT angiogram or coronary intervention is essential to rule out conditions causing pseudo-Wellens syndrome like pulmonary embolism, vasospastic angina, intoxication with cannabis and phencyclidine, or crack cocaine use 7.
Treatment of Wellens syndrome
Although Wellens syndrome is a well-known syndrome among the cardiologists, there is no guideline based management recommendations 5.
Left untreated 75% of patients with Wellens syndrome can progress to extensive anterior wall infarction 1 7.
Medical management is often not successful and immediate coronary intervention is recommended to prevent morbidity and mortality 1 5 7.
A timely diagnostic and therapeutic approach will be able to prevent a massive infarction in left anterior descending artery territory and reduce the high morbidity and mortality associated with coronary artery disease 2.
With definitive management of the stenosis, T wave changes resolve with normalization of the electrocardiogram 6.
Summary
Wellens syndrome includes a highly specific pattern of T wave changes in the anterior chest leads in patients with unstable angina. It has been associated with critical, proximal left anterior descending artery stenosis.
75% of patients with Wellens syndrome may progress to extensive anterior wall infarction, for this reason, it is important to recognize these EKG patterns and start the correct therapeutic procedure in the emergency department.
A timely diagnostic and therapeutic approach will be able to prevent a massive infarction in left anterior descending artery territory and reduce the high morbidity and mortality associated with coronary artery disease.
References
- 1. de Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982; 103 (4 Pt 2): 730-736. doi: 10.1016/0002-8703(82)90480-x.
- 2. Ramires TG, Sant’Anna J, et al. Wellens’ syndrome: a pattern to remember. BMJ Case Reports. 2018; bcr-2018-224582. doi 10.1136/bcr-2018-224582.
- 3. Parikh KS, Agarwal R, Mehrotra AK, Swamy RS. Wellens syndrome: a life-saving diagnosis. Am J Emerg Med. 2012 Jan; 30(1): 255.e3-5. doi: 10.1016/j.ajem.2010.10.014.
- 4. Miner B, Grigg WS, Hart EH. Wellens Syndrome. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. [cited: November 20, 2022]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482490/.
- 5. Ramanathan S, Soaly E, Cherian A, Heidous MA. ‘T’ twist: Wellens syndrome. QJM. 2019; 112: 373-374. doi: 10.1093/qjmed/hcy276.
- 6. Rhinehardt J, Brady WJ, et al. Electrocardiographic manifestations of Wellens' syndrome. Am J Emerg Med. 2002; 20:638–43. doi: 10.1053/ajem.2002.34800.
- 7. Mishra AK, Sahu KK et al. Wellens syndrome: Differential and outcome. QJM. 2019; 112: 825-826. doi: 10.1093/qjmed/hcz128.
If you Like it... Share it.