Abnormal Electrocardiogram Findings in Athletes
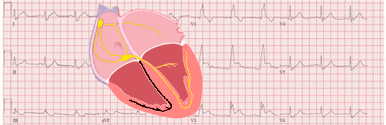
Electrocardiographic changes in athletes usually reflect benign structural and electrical remodelling of the heart as an adaptation to regular physical training (athlete's heart) 1 2.
But, in rare cases, abnormalities of an athlete’s EKG may be an expression of an underlying heart disease putting the athlete at risk of sudden cardiac death during sport 2.
It is imperative that EKG abnormalities resulting from intensive physical training and those potentially associated with an increased cardiovascular risk are properly defined.
The ability to identify an abnormality on the 12-lead EKG, suggestive of underlying cardiac disease associated with sudden cardiac death, is based on a good knowledge of the normal EKG characteristics within the athletic population 1.
Sudden Cardiac Death in Athletes
Cardiovascular-related sudden death is the leading cause of mortality in athletes during sport and exercise 1 3 4.
The majority of disorders associated with an increased risk of sudden cardiac death are suggested or identified by abnormalities on a resting 12-lead EKG 3.
Whether used for the evaluation of cardiovascular-related symptoms, a family history of inheritable cardiac disease or premature sudden cardiac death, or for screening of asymptomatic athletes, EKG interpretation is an essential skill for all physicians involved in the cardiovascular care of athletes.
An EKG increases the ability to detect underlying cardiovascular conditions that may increase the risk for sudden cardiac death. In most countries, there is a shortage of physician expertise in the interpretation of an athlete’s EKG.
Normal EKG Findings in Athletes
Related article: Normal EKG findings in athletes.
These training-related EKG alterations are physiologic adaptations to regular exercise, considered normal variants in athletes, and do not require further evaluation in asymptomatic athletes with no significant family history 1 3:
More information: Normal EKG findings in athletes.
Abnormal T Wave Inversion
Related articles: Left ventricular hypertrophy on the EKG, ARVC on the EKG.
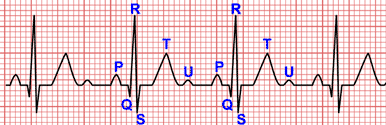
The presence of T wave inversion ≥1 mm in two or more contiguous leads (excluding leads aVR, III, and V1) in an anterior, lateral, inferolateral, or inferior territory is abnormal and should prompt further evaluation for underlying structural heart disease 3.
Normal exceptions include T wave inversion confined to leads V1–V4 in black athletes when preceded by J point and/or ST-segment elevation, and T wave inversion in leads V1–V3 in athletes under 16 years of age (juvenile T wave pattern) 3.
T wave inversion in lateral or inferolateral leads
T wave inversion in the lateral or inferolateral leads is often associated with the presence of quiescent cardiomyopathy in a considerable proportion of athletes 3 5.
This electrocardiographic finding should prompt a comprehensive investigation with an echocardiogram or cardiac magnetic resonance to exclude cardiomyopathy 6.
Exercise EKG testing and Holter monitoring also should be considered in the evaluation of lateral or inferolateral T wave inversion. The presence of ventricular tachycardia during exercise or Holter may support hypertrophic cardiomyopathy and is also useful in risk stratification 3.
T wave inversion in anterior leads
T wave inversion in anterior leads is a normal variant in asymptomatic adolescent athletes under 16 years of age, in black athletes when preceded by J-point elevation and convex ST-segment elevation, and in some endurance athletes 3.
However, T wave inversion in leads V1, V2 and/or V3 also is a recognized pattern in patients with arrhythmogenic right ventricular cardiomyopathy (ARVC) and rarely hypertrophic cardiomyopathy 3.
In most non-black athletes age ≥16 years, T wave inversion in anterior leads beyond lead V2 should prompt further evaluation given the potential overlap with ARVC.
Concurrent findings of J-point elevation, ST-segment elevation, or biphasic T waves more likely represents athlete’s heart, while the absence of J-point elevation or a coexistent depressed ST-segment is more concerning for ARVC.
Other EKG findings suggestive of ARVC include low limb lead voltages, prolonged S wave upstroke, ventricular ectopy with left bundle branch block morphology, and epsilon waves.
A combination of tests is needed to diagnose ARVC including echocardiography, cardiac MRI, Holter monitoring, exercise EKG test, and signal averaged EKG.
T wave inversion in inferior leads
The significance of T wave inversion confined to the inferior leads is unknown.
However, this finding cannot be attributed to physiological remodelling and thus warrants further investigation with, at minimum, an echocardiogram 3.
More information: Left ventricular hypertrophy on the EKG, ARVC on the EKG.
ST-Segment Depression
Related article: ST-segment analysis.
ST-segment depression is common among patients with cardiomyopathy but is not a feature of athletic training 3.
ST-segment depression in excess of 0.05 mV (0.5 mm) in two or more leads should be considered an abnormal finding requiring definitive evaluation for underlying structural heart disease 6.
Echocardiography is the minimum evaluation for athletes with ST-segment depression to investigate for underlying cardiomyopathy 3.
Cardiac MRI should be considered based on the echocardiographic findings or clinical suspicion 3.
More information: ST-segment analysis.
Abnormal Q Waves
Related article: The Q wave.
Several pathological disorders including hypertrophic cardiomyopathy, arrhythmogenic right ventricular cardiomyopathy, infiltrative myocardial diseases, accessory pathways and transmural myocardial infarction can lead to the development of exaggerated (deep or wide) Q waves or unexpected Q waves in atypical leads 3.
Pathological Q waves have been reported in approximately 1–2% of all athletes, and may be higher in males and black athletes 6.
For asymptomatic athletes, pathological Q waves were previously defined as >3 mm in depth or >40 ms in duration in two or more leads. In practice, however, this criterion is a common source of false positive EKG results.
Pathological Q waves in athletes are currently defined as a Q/R ratio ≥0.25 (25%) or ≥40 ms in duration in two or more contiguous leads (except in leads III and aVR) 3.
An EKG with abnormal Q waves should be carefully examined for the possibility of an accessory pathway.
Persistence of pathological Q waves in two or more contiguous leads warrants further investigation with echocardiography or cardiac MRI to exclude cardiomyopathy.
If the echocardiogram or cardiac MRI are normal and there are no other concerning clinical findings or EKG abnormalities, no additional testing is generally necessary 3.
In athletes over 30 years of age with suspicion of prior myocardial infarction or risk factors for ischemic heart disease, stress testing may be warranted 3.
More information: The Q wave.
Complete Left Bundle Branch Block
Related article: Left bundle branch block.
Left bundle branch block is found in less than 1 in 1000 athletes but is common in patients with cardiomyopathy and ischaemic heart disease 6.
Thus, complete left bundle branch block always should be considered an abnormal finding and requires a comprehensive evaluation to rule out a pathological cardiac disorder.
Athletes with complete left bundle branch block require a thorough investigation for myocardial disease including echocardiography and a cardiac MRI with perfusion study 3.
More information: Left bundle branch block.
Ventricular pre-excitation
Related article: Pre-excitation syndromes.
Ventricular pre-excitation is evident on the EKG as the Wolf-Parkinson-White pattern defined as a PR interval <120 ms, the presence of a delta wave (slurring of the initial QRS), and a QRS duration >120 ms.
The Wolf-Parkinson-White pattern occurs in up to 1 in 250 athletes. The presence of an accessory pathway can predispose an athlete to sudden death because rapid conduction of atrial fibrillation across the accessory pathway may result in ventricular fibrillation.
A short PR interval in isolation without a widened QRS or delta wave in an asymptomatic athlete should not be considered for further assessment 3.
Intermittent pre-excitation during sinus rhythm on a resting EKG, or a complete loss of pre-excitation at higher heart rates during an exercise stress test suggests a low-risk accessory pathway 3.
An echocardiogram also should be considered due to the association of Wolf-Parkinson-White syndrome with Ebstein’s anomaly and cardiomyopathy.
If non-invasive testing cannot confirm a low-risk pathway or is inconclusive, an electrophysiological study should be considered.
More information: Pre-excitation syndromes.
Prolonged QT interval
Congenital long QT syndrome is a potentially lethal, genetically mediated ventricular arrhythmia syndrome with the hallmark electrocardiographic feature of QT interval prolongation.
It is recommended that male athletes with a QTc greater than or equal to 470 ms and female athletes with a QTc interval greater than or equal to 480 ms undergo further evaluation for long QT syndrome to better balance false positive and false negative findings 3.
Brugada Type 1 pattern
Related article: Brugada syndrome.
Brugada syndrome is characterized by the distinctive Brugada EKG pattern which consists of a coved rSr’ pattern, ST-segment elevation ≥2 mm, and inversion of the terminal portion of the T wave in one or more right precordial leads V1, V2, positioned in the 2nd, 3rd or 4th intercostal space 7.
Although three types were described, only the type 1 Brugada pattern is now considered diagnostic 7.
The coved ST segment elevation in type 1 Brugada pattern results in a broad r’ and should be distinguishable from the upsloping ST-segment elevation of early repolarization in an athlete.
The type 1 Brugada EKG pattern should be investigated regardless of symptoms 3.
More information: Brugada syndrome.
Profound sinus bradycardia or first degree atrioventricular block
Sinus bradycardia and moderate prolongation of the PR interval (200–399 ms) are recognized features of athletic conditioning.
Although a resting heart rate ≤30 bpm or a PR interval ≥400 ms may be normal in a well-trained athlete, an exercise testing or ambulatory EKG monitor may be indicated 3.
High grade atrioventricular blocks
Related articles: Second degree AV block, complete AV block.
Type II second-degree AV block and third degree AV block are abnormal findings in athletes.
If type II second-degree AV block or complete AV block is detected, further evaluation includes an echocardiogram, ambulatory EKG monitor, and exercise EKG test. Referral to an electrophysiologist is essential 3.
More information: Second degree AV block, Complete AV block.
Multiple Premature Ventricular Complexes
Related article: Premature ventricular complexes.
Two or more premature ventricular complexes (PVCs) are uncommon and present in less than 1% of 12-lead EKGs in athletes.
Although multiple premature ventricular complexes are usually benign, their presence may be the hallmark of underlying heart disease 3.
PVCs originating from the right ventricular outflow tract (left bundle branch block patern and predominantly positive QRS complexes in inferior leads) are considered particularly benign when associated with a normal EKG, however this PVC morphology can also be present in patients with early arrhythmogenic right ventricular cardiomyopathy particularly when the QRS complex exceeds 160 ms 3.
Therefore, the finding of two or more PVCs on an EKG should prompt more extensive evaluation to exclude underlying structural heart disease.
At a minimum, an ambulatory Holter monitor, echocardiogram, and exercise stress test should be performed to exclude complex ventricular arrhythmias.
If the Holter and echocardiogram are normal and the PVCs suppress with exercise, no further evaluation is recommended for an asymptomatic athlete.
In athletes with ≥ 2000 PVCs per 24 hours or with episodes of non-sustained ventricular tachycardia, or with an increasing burden of ectopy during an exercise stress test, additional evaluation may include contrast-enhanced cardiac MRI and electrophysiology study 3.
More information: Premature ventricular complexes.
Supraventricular Tachyarrhythmias
Related articles: Supraventricular tachycardias, atrial fibrillation, atrial flutter.
Sinus tachycardia is the most common atrial tachyarrhythmia in athletes but is very rarely due to intrinsic cardiac disease.
Supraventricular tachycardias (SVT), atrial fibrillation, and atrial flutter are rarely seen on a resting EKG in athletes and require investigation 3.
Supraventricular tachyarrhythmias are rarely life threatening but can be associated with other conditions that can lead to sudden cardiac death, including long QT syndrome, Wolf-Parkinson-White syndrome, Brugada syndrome, myocarditis, congenital heart disease, and the cardiomyopathies.
In these patients, an echocardiogram, ambulatory ECG monitor, and exercise treadmill test should be completed 3.
Referral to an electrophysiologist may be indicated for consideration of electrophysiology study and ablation.
If atrial fibrillation or flutter is found, an echocardiogram should be completed to assess for structural heart disease and anti-coagulation considered based on CHA2DS2-VASc score 3.
More information: Supraventricular tachycardias, atrial fibrillation, atrial flutter.
Ventricular arrhythmias
Related article: Ventricular arrhythmias.
Ventricular couplets, triplets, and non-sustained ventricular tachycardia always require investigation as they can be a marker for underlying cardiac pathology or lead to sustained ventricular tachycardia which may cause sudden cardiac death.
If ventricular arrhythmias are seen, the evaluation should include a thorough family history, an echocardiogram to evaluate for structural heart disease, cardiac MRI to assess for ARVC or other cardiomyopathies, ambulatory EKG monitor and exercise EKG test 3.
Depending on these results, further evaluation may be needed including electrophysiology study or genetic testing 3.
More information: Ventricular arrhythmias.
Considerations in athletes over 30 years of age
In athletes over 30 years of age, ischemic heart disease is the most common cause of sudden cardiac death.
In addition, older athletes may be less fit compared with 20–30 years ago, increasing the possibility of underlying ischemic heart disease.
While resting EKG has a low sensitivity for ischemic heart disease, some EKG patterns may suggest underlying coronary artery disease such as T wave inversion, pathological Q waves, ST-segment depression, left or right bundle branch block, abnormal R wave progression, left anterior fascicular block, and atrial fibrillation 3.
The main role of a resting EKG in older athletes is to identify those athletes who may potentially be at high risk for coronary artery disease and warrant further testing.
Initial testing should include an exercise stress test, resting echocardiogram, and assessment of traditional risk factors for ischemic heart disease 3.
References
- 1. Drezner JA, Fischbach P, Froelicher V et al. Normal electrocardiographic findings: recognising physiological adaptations in athletes. Normal electrocardiographic findings: recognising physiological adaptations in athletes. Br J Sports Med. 2013; 47: 125-136. doi: 10.1136/bjsports-2012-092068.
- 2. Corrado D, Biffi A, Basso C, et al. 12-lead ECG in the athlete: physiological versus pathological abnormalities. Br J Sports Med. 2009; 43: 669-676. doi: 10.1136/bjsm.2008.054759.
- 3. Sharma S, Drezner JA, Baggish A. International recommendations for electrocardiographic interpretation in athletes. Eur Heart J. 2018. Apr;39(16): 1466–1480. doi: 10.1093/eurheartj/ehw631.
- 4. Harmon KG , Asif IM, Klossner D, Drezner JA. Incidence of sudden cardiac death in national collegiate athletic association athletes. Circulation2011;123:1594–1600. doi: 10.1161/CIRCULATIONAHA.110.004622.
- 5. Schnell F, Riding N, et al. Recognition and significance of pathological T-wave inversions in athletes. Circulation. 2015; 131: 165–173. doi: 10.1161/CIRCULATIONAHA.114.011038.
- 6. Drezner JA, Ackerman MJ, Anderson J et al. Electrocardiographic interpretation in athletes: the ‘Seattle Criteria’. Br J Sports Med 2013; 47: 122–124. doi: 10.1136/bjsports-2012-092067.
- 7. Derval N, Sha A, Jaïs P. Definition of Early Repolarization: A Tug of War. Circulation. 2011; 124: 2185-2186. doi: 10.1161/CIRCULATIONAHA.111.064063.
If you Like it... Share it.