Ventricular Tachycardias
Ventricular tachycardias (VT) are a group of arrhythmias within ventricular arrhythmias. They are characterized by the presence of three or more consecutive ventricular beats with a high heart rate.
The appearance of ventricular tachycardia, especially in patients with ischemic heart disease, continues to be an important problem in clinical practice and, together with ventricular fibrillation, is one of the main causes of sudden cardiac death, especially in patients with structural heart disease 1.
Mechanisms of ventricular tachycardia
Ventricular tachycardia can be generated by three mechanisms: reentry (the most frequent), abnormal automatism and triggered activity.
Reentry
It is the most common mechanism after a healed acute infarct or in the healing phase.
It is produced by a reentry mechanism in areas of viable myocardium surrounded by the scar caused by myocardial necrosis.
VT substrate begins to develop from two weeks after the infarction, persisting indefinitely.
Abnormal Automaticity
It is the main mechanism of VT during an acute coronary syndrome.
Acute ischemia may increase the tissue excitability, favoring the focal activity for abnormal automaticity in normal tissue and initiate ventricular tachycardia.
Triggered Activity
The triggered activity is defined by impulse initiation caused by afterdepolarizations 2.
Early afterdepolarization: it is the mechanism of the torsades de pointes associated with a long QT syndrome.
Delayed afterdepolarization: main mechanism of right ventricular outflow tract VT and VT induced by exercise 2.
Electrocardiographic Classification of Ventricular Tachycardia
- Non-sustained ventricular tachycardia: three or more beats in duration, terminating spontaneously in less than 30 s 3.
- Monomorphic: non-sustained VT with a single QRS morphology.
- Polymorphic: non-sustained VT with a changing QRS morphology.
- Sustained ventricular tachycardia: VT greater than 30 s in duration and/or requiring termination due to hemodynamic compromise in less than 30 s.
- Monomorphic: sustained VT with a stable single QRS morphology.
- Polymorphic: sustained VT with a changing or multiform QRS morphology.
- Bundle branch reentrant (BBR) tachycardia: VT due to re-entry involving the His-Purkinje system, usually with LBBB morphology; this usually occurs in the setting of cardiomyopathy.
- Bidirectional ventricular tachycardia: VT with a beat-to-beat alternans in the QRS frontal plane axis (precordial leads), often associated with digitalis toxicity.
- Torsade de pointes: VT associated with a long QT, and electrocardiographically characterized by twisting of the peaks of the QRS complexes around the isoelectric line during the arrhythmia 3.
Monomorphic Ventricular Tachycardia
Monomorphic ventricular tachycardia is characterized by three or more ectopic ventricular QRS complexes with a single QRS morphology.
If it lasts less than 30 seconds is called non-sustained ventricular tachycardia, if it lasts longer than 30 seconds or precise electrical cardioversion is called sustained ventricular tachycardia.
The main cause of monomorphic ventricular tachycardia is ischemic heart disease, especially the scar produced by a myocardial infarction.
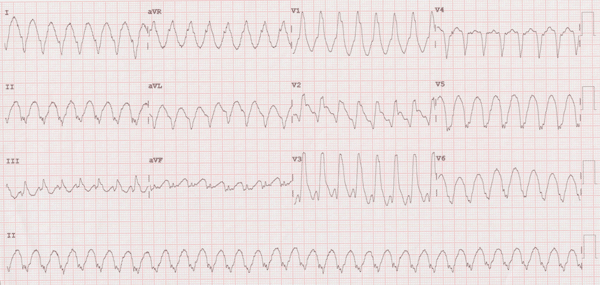
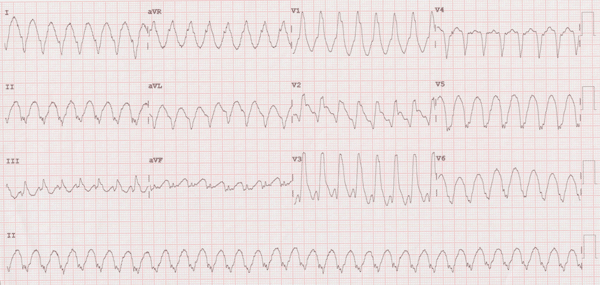
Monomorphic ventricular tachycardia: Wide QRS tachycardia at 188 bpm.
Electrocardiogram of Monomorphic Ventricular Tachycardia:
Related articles: Ventricular tachycardia criteria.
- High heart rate: ventricular rate is usually between 140 and 200 bpm. Although there may be monomorphic VT with a heart rate lower than 140 bpm.
- Ventricular QRS complex morphology: wide QRS complex in most cases. VT with narrow QRS complexes may be seen, but they are uncommon.
- Regular RR intervals: in up to 90% of cases, the intervals of the monomorphic ventricular tachycardias present a regular rhythm with similar R-R intervals.
- Onset of ventricular tachycardia: most VTs appear after a premature ventricular complex.
- AV dissociation: in patients with an underlying sinus rhythm, the atria may be stimulated by sinus node. So atrial and ventricular rhythms are independent, presenting dissociation between P waves and QRS complexes. This one of the most important diagnostic criteria for ventricular tachycardia 4.
More information: Ventricular tachycardia criteria.
Idiopathic Ventricular Tachycardias
Idiopathic ventricular tachycardia are a group of VT which appear in patients without structural cardiopathy.
- Outflow tract ventricular tachycardias: VTs which are predominantly localised in and around the right and left ventricular outflow tracts, and the aortic cusps.
- Fascicular left ventricular tachycardias.
- Ventricular tachycardias from the mitral annulus and from tricuspid annulus.
- Adrenergic ventricular tachycardia 5 6.
Bundle Branch Reentrant Tachycardia
The bundle branch reentrant tachycardia is a monomorphic VT associated with structural cardiopathy (dilated cardiomyopathy or severe valvular heart disease), and represents up to 6% of ventricular tachycardias 7.
In the basal electrocardiogram, it is common to observe disorders of the intraventricular conduction system, and during the VT, QRS with left bundle branch block pattern is observed in the majority of cases.
Ablation of the right bundle and definitive pacemaker implant is the the first line therapy 7.
Polymorphic Ventricular tachycardia
Polymorphic ventricular tachycardias present two or more different patterns of the QRS, and may or may not be associated with the presence of long QT.
The main cause of polymorphic ventricular tachycardia is ischemic heart disease especially acute myocardial infarction.
Polymorphic VT tends to degenerate into ventricular fibrillation and its treatment is the treatment of acute ischemia and electrical cardioverson if necessary.
Polymorphic Ventricular Tachycardia with Normal QT Interval
They are difficult to observe in clinical practice because they usually degenerate to ventricular fibrillation and sudden death.
The main cause of polymorphic VT with normal QT interval is ischemic heart disease, but it is also observed in patients with dilated or hypertrophic cardiomyopathy.
Polymorphic ventricular tachycardia also exists in patients with cardiac studies within normal limits, as in Brugada syndrome or catecholaminergic polymorphic VT.
Torsades de Pointes (Polymorphic VT with Long QT Interval)
Related article: Torsades de pointes.
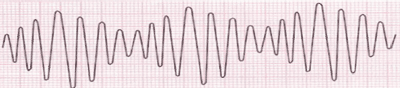
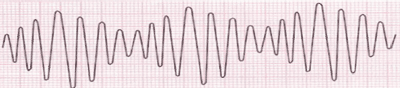
Electrocardiogram of torsades de pointes.
It is a type of polymorphic VT associated with the presence of long QT interval or increase in the amplitude of the U wave.
Electrocardiogram of Torsades de Pointes:
- Cycles of 5 to 20 beats of wide QRS tachycardia with HR around 200-250 bpm with irregular RR intervals.
- QRS complexes with a continuously turning heart axis, giving the impression that they "rotate" on the isoelectric line.
- It is usually initiated by a premature ventricular complex.
- In the complexes prior to or after the torsades de pointes a long QT interval is observed.
It is important to perform a 12-lead electrocardiogram for diagnosis, because in some isolated lead can be observed as a monomorphic VT, while in others it will have the typical torsades de pointes pattern.
Torsades de pointes often ends spontaneously but may degenerate into ventricular fibrillation and sudden death.
Polymorphic ventricular tachycardia with morphology similar to torsades de pointes but with normal QT interval should not be included in this definition.
More information: Torsades de pointes.
Bidirectional Ventricular Tachycardia
It is a very rare polymorphic ventricular tachycardia, which is associated with digitalis intoxication.
On the electrocardiogram, it is observed by the presence of a wide QRS complex tachycardia with an alternating shift in axis from one beat to another.
Alternating left and right bundle branch block patterns may be seen.
References
- 1. Benito B, Josephson ME. Ventricular Tachycardia in Coronary Artery Disease. Rev Esp Cardiol. 2012;65:939-55. doi: 10.1016/j.rec.2012.03.022
- 2. Gaztañaga L, Marchlinski FE, Betensky BP. Mechanisms of Cardiac Arrhythmias. Rev Esp Cardiol. 2012;65:174-85. doi: 10.1016/j.rec.2011.09.020.
- 3. Zipes DP, Camm AJ, Borggrefe M et al. ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death—Executive Summary. A Report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death). Circulation. 2006;114:1088-1132.
- 4. Surawicz B, Knilans TK. Chou’s electrocardiography in clinical practice, 6th ed. Philadelphia: Elservier; 2008.
- 5. Capulzini L, Brugada P, Brugada J, Brugada R. Arrhythmia and Right Heart Disease: From Genetic Basis to Clinical Practice. Rev Esp Cardiol. 2010;63:963-83.
- 6. Pérez-Diéz D, Brugada J. How to recognise and manage idiopathic ventricular tachycardia. E-journal for Cardiology Practice. 2010;8(26).
- 7. Caceres J, Jazayeri M, Mckinnie J, et al. Sustained bundle branch reentry as a mechanism of clinical tachycardia. Circulation 1989;79:256-70.