Torsades de Pointes
In 1966 François Dessertenne 1 reported the characteristics of the arrhythmia and proposed the French term torsades de pointes, this term means “twisting of the points”.
Torsades de pointes is a type of polymorphic ventricular tachycardia associated with QTc interval prolongation, it is characterized on the electrocardiogram (EKG) by a continuous twisting in QRS axis around an imaginary baseline 2.
Torsades de pointes usually terminates spontaneously but may degenerate into ventricular fibrillation.
Etiology of Torsades de Pointes
Torsades de pointes is associated with long QT interval which in the general population can be due to congenital or acquired long QT syndromes (LQTS). The incidence of acquired LQTS is much higher than the incidence of congenital LQTS 3.
Congenital LQTS has two genetic variants: Romano-Ward syndrome and Jervell and Lange-Nielsen syndrome.
There are many factors that predispose to QT prolongation including, e.g. age, female gender, left ventricular hypertrophy, heart failure, ischemic heart disease, hypertension, diabetes mellitus, hyperthyroidism, elevated serum cholesterol, hypokalemia, hypocalcemia, and hypomagnesemia 3.
However, one of the most common causes of acquired QTc prolongation is the use of specific drugs 3.
More than 50 medicines have been found to cause QT prolongations. Some common medicines that may cause the disorder include: antihistamines and decongestants, diuretics, antibiotics, anti-arrhythmic drugs, antidepressant and antipsychotic medicines, cholesterol-lowering medicines and some diabetes medicines.
Clinical Picture of Torsades de Pointes
Around 50% of patients with torsades de pointes are asymptomatic. The most common symptoms reported are dizziness, palpitations, hypotension, and syncope 4.
Sudden cardiac death is the presenting symptom in up to 10% of patients 4.
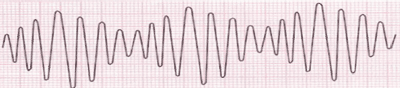
Torsades de Pointes on the electrocardiogram
The diagnosis of torsades de pointes is made based on the characteristic EKG findings.
It is important to record a 12-lead EKG for a correct diagnosis, because in some isolated lead can be observed as a monomorphic VT, while in others it will have the typical torsades de pointes pattern.
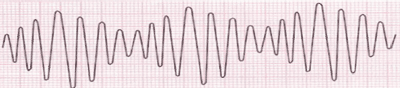
Electrocardiogram of torsades de pointes.
Electrocardiogram of Torsades de Pointes:
- Cycles of 5 to 20 beats of wide QRS tachycardia with rate around 200-240 bpm with irregular R-R intervals.
- QRS complexes with a continuously turning heart axis, giving the impression that they "twisting" around the isoelectric line.
- It is usually initiated by a premature ventricular complex.
- In the complexes prior to or after the torsades de pointes a long QT interval is observed.
Drug-induced torsades de pointes usually start with a short-long-short pattern of R-R cycles consisting of a short-coupled PVC followed by normal QRS after a compensatory pause (long R-R cycle), and then another PVC that typically falls close to the peak of the T wave 5.
Treatment of Torsades de Pointes
The first step in managing torsades de pointes is preventing its onset by targeting modifiable risk factors. This includes discontinuing any QT prolonging drugs and correcting hypokalemia, hypocalcemia, and hypomagnesemia 4.
Marked QT interval prolongation and torsades de pointes occur in 3 common settings: in congenital LQTS, in a drug-associated form, and in patients with advanced conduction system disease that has progressed to heart block.
Presentation with frequently recurring torsades de pointes in the congenital syndrome is unusual. In this setting, catecholamines should be avoided 6.
Torsades de pointes complicating heart block is managed with temporary pacing followed by permanent pacing 7.
However, other maneuvers useful in the drug-associated form (magnesium, potassium, pacing) can be used, and pacing along with beta blockade or lidocaine may be considered 6.
For patients with unstable torsades de pointes that does not terminate spontaneously or that degenerates into ventricular fibrillation, immediate high-energy unsynchronized shocks at defibrillation doses should be performed 5 6.
References
- 1. Dessertenne F. La tachycardie ventriculaire à deux foyers opposés variables. Arch Mal Coeur 1966;59:263-272.
- 2. Napolitano C, Priori SG, Schwartz PJ. Torsade de Pointes. Drugs. 1994; 47(1): 51-65. doi: 10.2165/00003495-199447010-00004
- 3. Van Noord Ch, Eijgelsheim M, Stricker BHCh. Drug- and non-drug-associated QT interval prolongation. Br J Clin Pharmacol. 2010 Jul; 70(1): 16–23. 10.1111/j.1365-2125.2010.03660.x
- 4. Cohagan B, Brandis D. Torsade de Pointes. [Updated 2019 Feb 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: www.ncbi.nlm.nih.gov/books/NBK459388/.
- 5. Drew BJ, Ackerman MJ, Funk M, et al. Prevention of torsade de pointes in hospital settings: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. Circulation. 2010;121(8):1047–1060. doi: 10.1161/CIRCULATIONAHA.109.192704
- 6. Zipes DP, Camm AJ, Borggrefe M et al. ACC/AHA/ESC 2006 Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death—Executive Summary. A Report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines. Circulation. 2006;114:1088-1132. doi: 10.1161/CIRCULATIONAHA.106.178233